UPDATE:
Group experiments are currently being set up at Mount Sinai hospital to test the Cool Fat Burner’s effects on blood glucose levels!
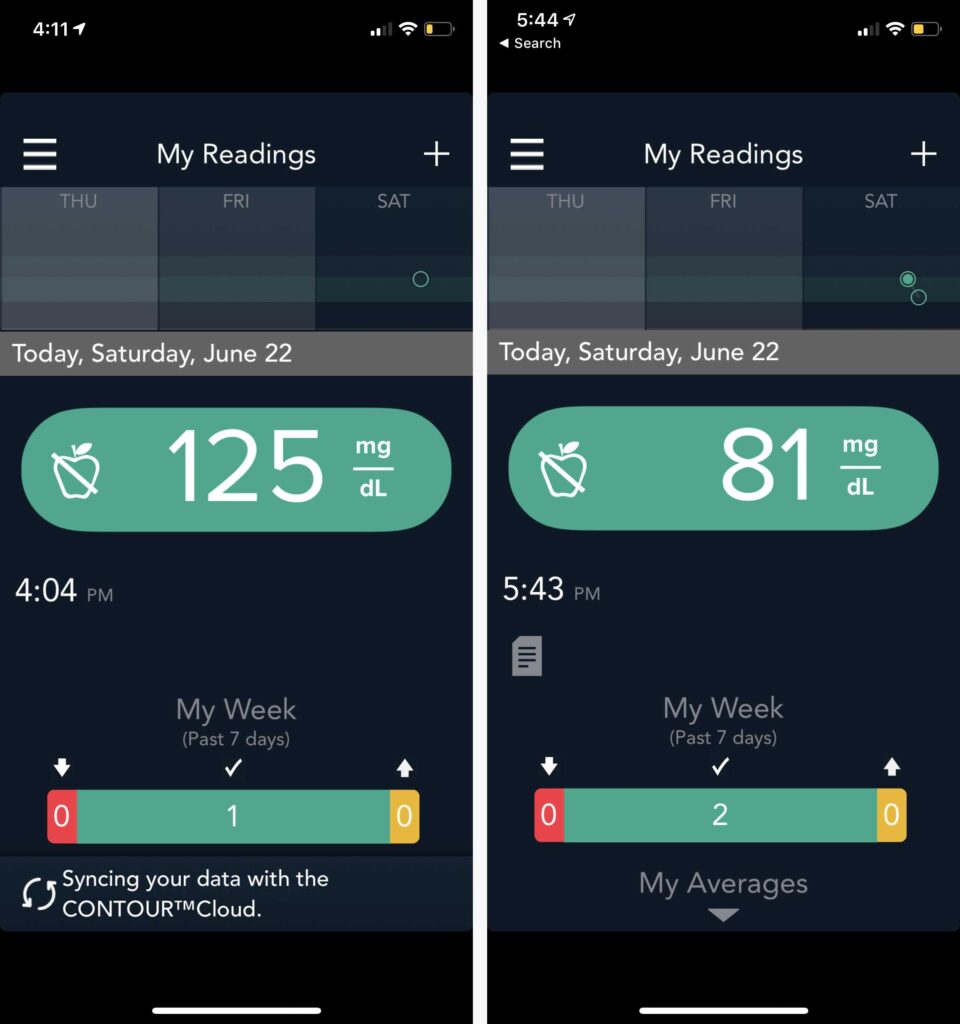
Update 2: metrics sent to us from a CFB customer — we get feedback like this all the time:
Background:
Not only is the Cool Fat Burner vest the first ever commercial Brown Fat, thermal loading, cold thermogenesis weight-loss device… it’s now shown to be able to burn off and lower one’s glucose levels in a single session, and can possibly help increase one’s insulin sensitivity over time. This has ramifications far beyond merely burning off calories and fat! Controlling blood glucose levels could be part of a plan to help improve health, rebalance hormones, and help treat everything from Type 2 diabetes to heart disease and other elements of the “metabolic disorder” resulting from chronically high glucose levels. *Results may vary.
Experiment design:
— Taper off and eventually stop all CFB use and exercise for several months. Fatten up and let my health deteriorate.
— Eat garbage every day, whenever I feel like it. (wholeheartedly partake in all holiday snacks and foods)
— The goal was to lose the insulin sensitivity that I had built up, evidenced by my cold-adapted, in-shape pic shown in the blog entry below.
— Gain weight.
— Start the experiment.
— Test glucose levels throughout the day.
— Get a baseline of elevated glucose levels, and for fasted levels. Do it enough to find the “normal” levels.
— Then add exercise and the Cool Fat Burner to that state of raised blood sugar and fasted blood sugar, and see what happens.
— Maintain the experiment for at least a month (glucose measurements spanned 48 days) to see if any insulin sensitivity returned. (this was not an initial goal, but occurred as insulin sensitivity quickly returned)
Questions:
— Does exercise lower glucose levels if they are raised (after meals)? What about if fasted? How much?
— Does cold thermogenesis with the Cool Fat Burner (at a near-to-full shiver state) lower glucose as well?
— And what changes in overall insulin sensitivity, if any, occur over the duration of the experiment?
Quick Refresher on Glucose and Insulin Sensitivity:
When you eat food, especially carbohydrates, that food is broken down into various “sugar” molecules (called glucose, fructose, and sucrose) in your digestive track. Those molecules pass into your bloodstream. Your body likes balance (called “homeostasis”). That includes blood sugar (glucose) levels that are too high or too low. So when you eat, it goes “too high.” Your body needs to bring it back down.
To lower your blood sugar, your body releases insulin from the pancreas. Insulin allows the glucose to pass into the cells of your brain, organs, and muscle to be properly stored or used up as fuel. This process lowers your blood sugar levels and brings it back to normal. But if that glucose does not get used up… it will then be stored as fat tissue… and if it’s chronically too high, it can lead to obesity, immune dysfunction, and various diseases such as Type II diabetes, cardiovascular disease, and possibly dementia related disorders such as Alzheimer’s.
If your glucose and thus insulin, is chronically too high… the insulin receptors on the various target cells (of the brain, organs, and muscles) will, over time, start to reduce in number. They make it harder for glucose to get in, because they’re constantly getting too much insulin/glucose… so they adapt by decreasing the “gatekeeper” receptors, trying to keep the overall amount of glucose entering the cells lower (trying to get it back to the normal level, compared to the elevated amounts.)
So when your body cannot properly respond to insulin, cannot properly pull glucose (blood sugar) into your organs and muscle to be used as fuel… your body has become insensitive to insulin. It no longer reacts to insulin by burning up that extra blood glucose. Instead, the extra glucose gets stored as fat, or floats around and increases systemic inflammation, ultimately leading to the metabolic disorders.
 |
What could lead to insulin insensitivity? — Genetics |
(Note: a variety of things can influence blood glucose levels. In an experiment such as this, it’s nearly impossible to rule out all factors, or get exacting data. Keep that in mind. All postprandial (after eating) readings were taken ~ 1 to 1.5hrs after. Same as post exercise and post Cool Fat Burner sessions.)
So here’s me, at the beginning, cold adapted in September. Around 3 months later the second pic is in December after fattening up a little.
September: “Before,” cold-adapted and highly insulin sensitive. Waistline at 31 ¾ inches.
Early December: After fattening up, losing some insulin sensitivity. Waistline at 34 ¼ inches.
So, starting out… Here’s the data, via glucose blood samples:
On occasion, my BGL would drop dramatically. For example, a night of partying (alcohol) with little food, had my BGL at 94, but the next morning it was down to 86.
This was all during the first few weeks.
If I fasted and didn’t eat simple carbs, my BGL could eventually lower and stay in the 80’s, especially over the next few weeks, as the CFB and exercise sessions added up and insulin sensitivity began to return.
BGL: 99
The next morning. 9-10hrs after eating.
|
|||||||||||||||||
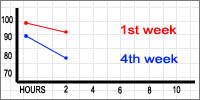
4th week —Before: 99
After: 94
Dropped 5ptsBefore: 89
After: 77
Dropped 12pts 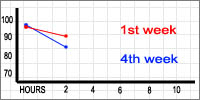
4th week —Before: 96
After: 92
Dropped 4ptsBefore: 98
After: 87
Dropped 11pts
Conclusions & Discussion:
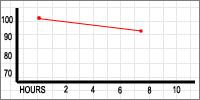
— Steady-state endurance (jogging for 55 minutes) and cold thermogenesis (Cool Fat Burner at near-shivering intensity for ~ 1.5hrs) lowered blood glucose levels, when those levels are elevated due to ingestion of simple carbohydrate.
— In the first few weeks, both activities lowered BGL around 4-5pts. By the fourth week, they lowered levels by 11-12pts.
— As the experiment went on, keeping BGL up became more and more difficult.
This blog entry is only a brief summary of the whole experiment. I took glucose readings at morning and noon fasting, as well as before and after meals. Readings were taken before and after resistance training, power endurance work, steady-state cardio, and distance running. And before and after using the Cool Fat Burner, at different intensities, as well as days with no activity whatsoever. I tried to take readings 1-1.5hrs after meals and activity. (I went though over 150 glucose test strips)
None of those activities really lowered fasting glucose levels consistently.
This is not unexpected. Ideally, with ‘healthy’ glucose levels, your body prefers to burn fat and glycogen, instead of glucose, during cold thermogenesis. This study shows that cold exposure burns energy ratios of 50% fat, 30% glycogen, only 10% glucose, and 10% protein. So when one’s glucose is high, like after eating junk food, the Cool Fat Burner will likely cause the body to burn that extra glucose to generate heat, more so than using glycogen and fat. (Since BAT is more active in the fasted state, it’s also possible that muscle tissue (uncoupling, sarcolopin) more so than BAT, actively burns up that extra glucose during higher-glucose-level thermal loading.) If one’s glucose is at healthier levels, as one should see in healthy insulin sensitivity (probably in the 80’s for most) cold thermogenesis will activate BAT, which will burn higher levels of fat (50%) and glycogen (30%).
At the beginning of the experiment, during the first few weeks, it took very little junk food to raise my blood glucose levels. And they stayed up. By the fourth week, I had to eat more and more junk food, along with fiber, to keep my BGL up for more than an hour or two; in other words, my insulin sensitivity was returning. My BGL would drop on it’s own accord if I didn’t eat the fiber and solid foods. I even resorted to taking metamucil fiber supplement with meals to keep the BGL from falling too quick.
By the end of the experiment (around 48 days) I could no longer keep my BGL up, no matter how much garbage I ate, no matter how much fiber I ate with it. My body once again became responsive to insulin, and began properly using up the glucose, at least in comparison to where I was at the start.
I was only able to jog twice. After the first time, my foot was injured. After the second run (fourth week) my knee was aching. One could argue that in itself has implications. (Also, this was during winter; I tried to dress warmly, but there could have been some thermal loading in effect during jogging even just from sucking down cold air)
Resistance and power endurance training elevated fasting BGL (starting in the 80’s) often to over 100. It would go back down later, at least towards the end of the experimental period. This is a common response to resistance training. Steady state “aerobics” (45 min, heart rate around 60-75%) had little effect on BGL, though again, those were during fasted training sessions.
It’s ridiculous the amount of things that can influence one’s blood glucose levels. The smallest amount of the right (or wrong?) type of food can have a huge impact and shoot it up.
I imagine the overall quick return of insulin sensitivity was a combined result of intermittent fasting eating schedule, exercise, and cold thermogenesis. Each played a part. (I exercised and used the CFB ~ 2 to 3 alternating days each, a total of 5-6 per week. I did an IF schedule (usually 18/6) probably 4 days a week.) It’s also likely that I didn’t really lose all insulin sensitivity in the few months I “fattened up.” I wasn’t starting from scratch, I just had to reestablish what I’d temporarily blunted via poor diet and living. Nevertheless, my BGL during the first week or so were in line with someone theoretically at risk for Type II diabetes, in that it would often be over 100, and would stay relatively high for hours and hours.